I have never written about my 23-year battle with prostate cancer. It’s been an egg too fragile. But I was inspired to write about it after my friend Bill Williams sent a link to an NPR Fresh Air podcast describing the time when Salman Rushdie was on stage in 2022 at a literary event in upstate New York when he was attacked by a man in the audience with a knife. In his words:
"Dying in the company of strangers — that was what was going through my mind."
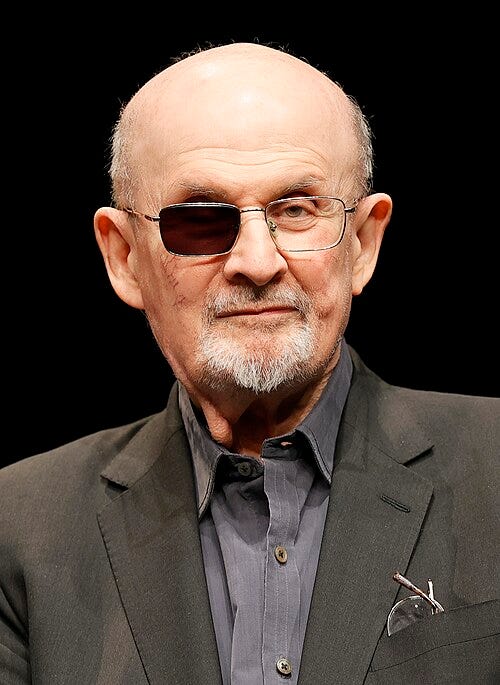
Salman Rushdie is an Indian-born, British and American novelist. After his fourth novel, The Satanic Verses (1988), Rushdie became the subject of several assassination attempts and death threats, including a fatwa calling for his death issued by Ruhollah Khomeini, the leader of Iran. The Japanese translator of the book, Hitoshi Igarashi was stabbed to death in 1991. It was the recipient of several book awards, and was seen as the most ambitious novel published at the time that dealt with the immigrant experience in Britain. His latest book Knife speaks to the attack. When Rushdie was asked if the writing of the book had therapeutic value he quoted another author who said, “Only write books you can’t avoid writing.” While my essay here is not a book, I guess it follows that logic. Mine is a narrative that allows me to reflect on and recall what the human body can endure with the proper dose of determination. Salman describes that determination as key to his ability to endure his own private hell.
I am in no way comparing my experience to Mr. Rushdie’s. His was an instantaneous horrifying event that he describes as a piñata being knifed many times by a madman. It took seven weeks of hospitalization and the skills of many specialists. My own journey has been a roller coaster of hope, trials, and treatments that, in many ways, has echoed some of the emotional trauma that Salman experienced.
It all started in November of 2002 at the age of 62. At a routine checkup I had a 4.2 PSA reading which normally would not raise eyebrows. PSA is a test that measures the amount of prostate specific antigen in your blood, a principal marker for detecting prostate cancer. But since my reading was borderline, a “free PSA” test was given. Without getting too deep in medical esoterica, the “free” part gives a more definitive take on things—a test that in this case sent me to the next level of investigation: a biopsy. Bingo! On December 9th of ‘02 a probe of the prostate indicated cancer in five out of six core samples, plus a 4+4 Gleason score, or 8, with 10 being the worst. This indicated a high-grade cancer. When I was shown a picture of a cross section of the cell it looked like a war between amoebas. In other words, it was a highly disorganized mass whereas the masses with better behavior—better organized—are less dangerous. Kind of like an unruly classroom versus one that is well-behaved.
When the doctor presented me with the news it was just before Christmas of 2002. As those who get a cancer prognosis will tell you, it takes the air out of your lungs. Your thinking immediately gravitates to the dark side. After an anguished mulling of the options and in concurrence with my family’s and doctors’ thinking, I decided to have a Radical Prostatectomy, a surgery to totally remove the prostate and several adjoining lymph nodes. I wanted it out! So, on February 23rd, 2003, Dr. Peter Carroll at UCSF performed the surgery. All went well and there was no sign of any rebel cells outside the fascia (external skin). Dr. Carroll originally organized the Urologic Oncology Service at UCSF and is a Professor of Urology. He is not only a gifted surgeon and doctor but a very approachable, bright, and warm human being. We still keep in touch all these years later.
The post-op PSA was low but began rising for the next four years. It was climbing enough so that in 2004 they started me on Lupron, a synthetic hormone that reduces testosterone and slows cancer growth. Of course there are always side effects: I had hot flashes and night sweats, although not as bad as other prostate cancer patients. They also started me on Casodex, another type of hormone therapy with its own side effects. In August of that year I had my first round of radiation therapy just to throw something else at it since the PSA was not to the doctors’ liking. Then, things started to go in the wrong direction with a rising PSA by the latter part of 2010. The Lupron and Casodex were administered off and on through early 2014.
By May of 2014 a PET scan of my bones showed some small lesions forming along with more increases in the PSA. In July I was put on a double-blind clinical trial called ARN-509, a study for improving non-metastatic prostate cancer. I was on this while on a tour of Turkey with my wife. While I found the sites we visited there fascinating, I was distracted by my thoughts about what this drug might be doing. Later, I found that I was on the placebo, meaning that I wasn’t receiving whatever benefits may have accrued from the real drug.
By the end of October, 2015, my PSA had shot up to over 18. Enter Xtandi (Enzalutamide), a drug that is used for patients that have a high risk of their cancer spreading to other parts of the body. This brought the PSA down but not low enough. PET and CT scans showed more issues, with uptake of the contrast fluid to lesions in my ribs. Sleep was becoming more difficult not knowing what lay ahead.
At the end of January, 2017, another round of radiation, this time IMRT or Intensity Modulated Radiation Therapy. Then, hopeful thoughts until May of 2018 when I experienced four days of nausea, vomiting, and diarrhea, requiring a visit to the ER. With some CTs showing metastases, several sessions of radiation ensued targeting ribs, neck, and lungs into February of 2018.
Intermission
Phew! This is hard work—for the reader as well as the author. Let’s just take a moment to reflect on something Salman Rushdie said after his horrible incident. He said that he now has a new relationship with his body. When I reflected on that comment, I began to wonder whether our bodies do indeed have personalities of their own. It’s possible that I now respect and admire my own body for what it has endured; this would include other surgeries over time: shoulder, hernia, sinus, cataracts, vasectomy, tonsillectomy and adenoidectomy as a child (I came close to folding my cards after those last two), dental, femurs, and spinal.
For those who are still with me, it gets more interesting. The PSA continued its march until even more “stuff” was showing up on the CT scans. Next: a decision to give stereotactic body radiotherapy (SBRT), a precise, high-dose form of radiation therapy that allows physicians to treat cancer in just one to five treatments, rather than the multiple doses over many weeks required in conventional radiation. These were delivered to a rib, a lung, and neck nodes.
Yet another visit to the ER in November, 2019, with an upper respiratory infection, pneumonia, shortness of breath and fatigue. These problems have since been recurring themes with me and relate to a weakening of the immune system caused by the many cancer treatments. By August of 2020, things were heating up. A PSMA PET scan showed an advanced spread of the cancer. On a PET scan, "uptake" refers to the amount of a radioactive tracer absorbed by tissues or cells. Some mild fractures were beginning to show. I had been on a drug called Enzalutamide, or Xtandi, to treat patients who have metastatic prostate cancer. At that point metastatic lesions had filled the full diameter of my femurs (upper leg bones). Because I was then at risk for pathologic failure (i.e., broken bones), it was decided to surgically place titanium rods in both of my femurs—within three days of each other. I had the good fortune to have another top flight UCSF surgeon, Dr. Melissa Zimel who deals with orthopedic oncology. Dr. Zimel is not only a very skilled surgeon but a delightful and calming presence in the operating room.
A PSA of over 20 made me a candidate for yet another clinical trial, Keynote-921. By January of 2021 my PSA had risen to 30. More trips to the ER for various reasons. An MRI of the spine showed fractures of the L2 and L4 vertebrae and then metastatic prostate adenocarcinoma, a spread of the cancer throughout the body. A lesion was now pressing into the spinal column and compressing the spinal fluid. This was decision time. Things were looking grayer all the time. The choices were between more radiation or surgery to remove the lesion. At one point consideration was given to emergency spinal surgery. About this time, I was lucky enough to get referred to Dr. Praveen Mummaneni who is the co-director of the UCSF Spine Center and vice chair of the neurosurgery department. He has been selected by U.S. News & World Report as one of the best doctors in the nation every year since 2005. In other words, I was in great hands for a very delicate procedure. He performed a spinal fusion of T12-L4 with bone cement augmentation of L2 and L4. Rods, screws, and bars were placed for rigidity. I always say it’s like owning an aisle in the local hardware store. Bottom line: this operation was a life saver.
While the surgery was successful, I was immobile and in considerable pain. This meant three weeks in the CPMC acute rehab department of the Ralph K. Davies Medical Center. At first, I couldn’t even get to the bathroom. I was loaded into a sling that was hooked up to a track system in the ceiling. This sounds like a lot of fun but it was painful. I couldn’t help but think about the historic transit system, the monorail in Wuppertal, Germany, that still zips around on a suspended rail. The folks at Davies were amazing in getting me back as a functioning human being. No wonder they call it the Boot Camp. Non-stop daily activities and exercises were not only done with purpose and rigor, but also with compassion. I was discharged in February of 2022.
In May of 2022 I fell, which was diagnosed as the result of pneumonia (what else?) and pleural effusion which is a build up of fluid between the layers of tissue that line the lungs and chest cavity. When I hit a wall with my head I was left with a small fracture where the skull meets the spine. They insisted on giving me one of those bulky neck braces. I wore it three times and only once in public. I said that I was pretty certain that my head wasn’t going to fall off. My attempt at humor was underappreciated.
By mid-May of ‘22, both my PSA and metastases were increasing pretty dramatically. Traces of the cancer were now found pretty much everywhere—ribs, bones, spinal column, lymph nodes, and abdomen. My PSA rose from 70 on May 11 to 94 on June 6. I was started on Keytruda (Pembrolizumab), a type of immunotherapy. This caused acute respiratory distress bringing on another round of shortness of breath and pneumonia. By June 21, my PSA had increased to 153, and then to 210 by July 6.
To make things even more interesting, I acquired a mean case of shingles in October of ‘23. After some delay in diagnosis and acute weakness, it was discovered that I had sepsis, a potentially fatal blood disease. Large doses of antibiotics finally corralled the extent of the condition and I was released from isolation in the hospital. I had had the two-part dosage of the vaccine, but at least that may have prevented a more serious case. I still have nerve sensitivity around my hip where the infection seemed to have had its headquarters.
Help is on the way
For some time my wife Peggy and I had been following the potential use of a drug called PSMA-lu or Pluvicto by Novartis. We had heard good things about it but, after all the treatments to date, false hopes and frustrations ruled my mind. In order to qualify for the drug you had to have prostate-specific membrane antigen–positive metastatic castration-resistant prostate cancer. In shorthand you had to have prostate cancer that has spread beyond the prostate and metastasized after treatments with other therapies: hormonal, chemotherapy, and radiation. Basically, you’ve tried everything. A while back I had chemo sessions for ten weeks which was 4 sessions more than they normally give. These were increasingly brutal and kept me in bed for periods at a time. It also left me with neuropathy in my feet which, to this day, still affects my walking. I just had my first experimental laser treatment of the feet to minimize the sensitivity and pain of the neuropathy.
Dr. Thomas Hope, a professor of radiology at UCSF, guides the Pluvicto program. In mid-2023, he scheduled a PSMA PET scan which showed that I had very high potential for successful treatment under the Pluvicto drug. The scan showed black patches (lesions) throughout my body—not a pretty picture. I was indeed a prime candidate. The drug is administered once a week over six weeks. I had my first dose in July of 2023 and my second one in August of that year. By December, I had a non-detectable PSA. I continue to be the poster boy for the Pluvicto drug at UCSF. This means that my cancer is in remission and I have another four treatments remaining should I need them (I call it money in the bank). Dr. Hope reminds me that my cancer could return (doctors unfortunately have to give all sides). In the meantime, I am enjoying an incredible run, roughly 19-months-long since my last treatment.
During this overall 23-year period I also had innumerable PET and CT scans, MRIs, injections, and blood draws—too many to itemize, fortunately for the reader.
My support team
Back to Salman Rushdie. One of his points was the role his American wife played. During his seven weeks of hospitalization and beyond, Rachel Eliza Griffiths, herself an accomplished poet, novelist, visual artist, and photographer, basically had to modify her lifestyle and become supporter, caregiver, and advocate for her husband after the attempt on his life.
My wife Peggy, over a period of the last 23 years has, on innumerable occasions, played morale booster, caregiver, advisor, and confidant. That period represents forty percent of our married life. She was present with me in physician meetings where critical decisions were being made and quite often at my side in the hospital. There is no amount of thanks that can repay her devotion and loving support.
My daughter Margot frequently acted as a key supporter and on many occasions helped prepare my travel bag to take to the hospital (my frequent visits required a packing list). She made sacrifices in both her career and social life to accommodate many a last minute rush to the ER. Her calming influence helped smooth out the often rough periods.
My son Peter would, on occasion, come up from Southern California and spend quality time with me. His presence helped take the pressure off other family members.
There have been too many doctors to mention that attended to me over this time period. I have been blessed with the finest and most professional medical personnel around. I just hope I don’t need their services again in the near future.

Jack,
i had no idea you went through all of this.
Reading this, the last thing I expected was that good news ending. Wow. (I’ve been on the PSA … biopsy … waiting … PSA… hamster-wheel for about five years.